International researchers collaborate to understand trends in blood product use
Thursday, November 02, 2017 Dr. Kendra Hodgkinson
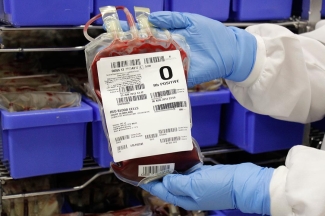
Canadian Blood Services currently has a special need for O-negative donors. And we aren’t alone — many blood operators worldwide have recently increased their efforts to recruit O-negative blood donors.
Why are O-negative donors in such high demand?
Matched (or group specific) blood is always preferred for transfusion; however, O-negative blood can be transfused to recipients who have any ABO blood type (A, B, AB or O) and Rh type (positive or negative). This makes them vital for emergency transfusions when the recipient’s blood type is unknown, or if ABO-matched and/or Rh-matched blood products are unavailable for a patient in need.
Inventory management is a daily challenge for blood operators and hospitals to ensure adequate supply of each blood type so that any patient at any time can be safely transfused. Maintaining an adequate inventory of O negative blood can be even more challenging for the following reasons:
- Challenge #1: Red blood cell products are manufactured from whole blood collected from donors (yes – volunteer donors) and only 7 per cent of Canadians are O-negative. While blood operators specifically target this small donor population, there are not many of them and, for their safety, there are limitations to how often they can donate.
- Challenge #2: Red blood cell products can only be stored for 42 days (yes – the eggs in your fridge might last longer!), so the need to collect is ongoing.
- Challenge #3: While improved transfusion practice in hospitals is leading to an overall decline in red blood cell utilization (yes – physicians are transfusing less), we are only starting to appreciate the important nuances of this decline and how they impact inventory management.
- Challenge #4: Many transfusions are done in emergency situations, when the blood type of the recipient is often unknown. Large quantities of O-negative blood are sometimes needed to save the lives of these patients.
Read more about how hospital blood banks manage their blood product inventory in "Not Your Average Bank"
How is research shedding light on red blood cell inventory?
Researchers at our Centre for Innovation are working with international colleagues to better understand the patterns of red blood cell distribution and use. Studies like these can help inform health-care providers worldwide about the optimal donor collection strategy and the distribution and use of O-negative blood products, reducing the risk of shortages in the future.
In a long term Trends for Collection (TFC) study, an international group of researchers that included Canadian Blood Services’ chief medical and scientific officer, Dr. Dana Devine, compared the numbers of red blood cells distributed to hospitals by blood services in several countries including Canada. They found that blood centers are distributing less red blood cells to hospitals and that this may be attributed to the excellent Patient Blood Management programs implemented in hospitals. However, this downward trend is not the same for all blood types. In fact, the proportion of O-negative blood distributed to hospitals increased during the same period. The reasons for this were not examined in this study, but could be caused by factors such as hospitals’ desire to maintain a flexible inventory or a possible increased use in emergency transfusion.
Dr. Michelle Zeller, a medical officer at Canadian Blood Services, and Prof. Nancy Heddle, one of our adjunct scientists, collaborated with Canadian and international researchers to determine why Type O blood is being used more often. Dr. Zeller and Prof. Heddle are part of the McMaster Centre for Transfusion Research, which is supported by the Centre for Innovation. Their GRoup O Utilization Patterns (GROUP) study surveyed hospitals in 11 countries and showed that a large percentage of O-negative blood products are used for patients who are not O-negative. Interestingly, this percentage varied at different sites, suggesting that hospitals with higher use of O-negative blood might be able to alter their policies to decrease non-essential use of this precious resource.
What is the research impact?
While the GROUP study was being undertaken, five participating sites re-evaluated their policy of giving O-negative blood to all patients with unknown blood type in an emergency setting, and implemented new policies to decrease their use of O-negative blood.
What is BEST?
Both of these studies were carried out in collaboration with the Biomedical Excellence for Safer Transfusion (BEST) Collaborative, an international research organization that aims to improve the safety of transfusion around the world. Canadian Blood Services is an active partner with the BEST Collaborative and this year our researchers have contributed to 9 of the 15 papers published by BEST. International studies allow “big-data” analysis of complex systems. Hospital and blood service policies may differ greatly between countries, allowing researchers to identify which policies are best for patient safety and for more efficient inventory management.
Other recent studies from Centre for Innovation researchers in collaboration with BEST:
- An international investigation into AB plasma administration in hospitals: how many AB plasma units were infused? The HABSWIN study.
- Comparison of donor and general population demographics over time: A BEST collaborative group study
- Prothrombin complex concentrate for emergent reversal of warfarin: an international survey of hospital protocols
- An international survey on the role of the hospital transfusion committee
- Impact of technical and assay variation on reporting of hemolysis in stored red blood cell products
- Quality control of apheresis platelets: A multicentre study to evaluate factors that can influence pH measurement
- Alternatives in blood operations when choosing non-DEHP bags
- Blood group antigen matching influence on gestational outcomes (AMIGO) study
Canadian Blood Services – Driving world-class innovation
Through discovery, development and applied research, Canadian Blood Services drives world-class innovation in blood transfusion, cellular therapy and transplantation—bringing clarity and insight to an increasingly complex healthcare future. Our dedicated research team and extended network of partners engage in exploratory and applied research to create new knowledge, inform and enhance best practices, contribute to the development of new services and technologies, and build capacity through training and collaboration. Find out more about our research impact.
The opinions reflected in this post are those of the author and do not necessarily reflect the opinions of Canadian Blood Services nor do they reflect the views of Health Canada or any other funding agency.
Related blog posts
In this six-part series, Dr. Jeannie Callum, a hospital-based transfusion specialist, shares her real-life experience witnessing the impact of blood donation on patient lives. She provides some fascinating insight into blood transfusion, past and present, and emphasizes the need for male donors and why some donors may be safer for patients.
Part 2 in a six-part series by Dr. Jeannie Callum, a hospital-based transfusion specialist who shares her real-life experience witnessing the impact of blood donation on patient lives. Here she provides some fascinating insight into blood transfusion, past and present, and emphasizes the need for male donors and why some donors may be safer for patients.
