Making decisions the right way – a global endeavour – Part 1
Wednesday, December 14, 2016 Jenny Ryan
Canadian Blood Services helped develop a unique framework for blood operators around the world to help improve and standardize the decision-making process when it comes blood safety.
The Alliance of Blood Operators (ABO) — an international body comprised of blood service organizations from around the world, Canadian Blood Services among them — has built a unique framework to help blood service operators streamline the decision-making process and make responsible decisions that lead to the greatest good.
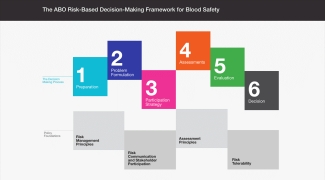
The framework helps organise and simplify the decision-making process by breaking it down into a series of logical and manageable steps.
Operational since 2015, many blood operators have used the risk-based decision-making framework for blood safety to make decisions around various aspects of blood collection, including donor eligibility factors, risk mitigation and testing protocols.
An interview with Judie Leach Bennett, director of Canadian Blood Services' Centre for Innovation
What is the risk-based decision-making framework?
The risk-based decision-making framework was designed to help blood operators optimize their blood-safety decision-making. The Alliance of Blood Operators (ABO) led an effort to create a new framework that would help blood operators with the decision-making process, to allocate finite resources to where the greatest risk is, and finally to account for all those factors that surround the medical and scientific issues, such as economic, social, and ethical concerns.
Can you give me a bit of background about how it was developed and who was involved?
In 2010, the ABO held a consensus conference. It was an international conference on risk-based decision-making in the context of blood safety. The need for a new decision-making paradigm was called out. In response, the ABO decided to create this framework.
It was developed over the course of 2013-2015. At first, we looked at various frameworks that existed and then did the work to develop a framework that would fit the blood operator context.
Why do you think that blood operators needed a framework like this to make decisions?
We have all made decisions up to now … very good decisions. But, with this framework we can all make decisions in a very structured way, in an evidence-based way, and in a way that looks at the proportionality between mitigation and the risk. We can also look at opportunity cost of that mitigation, while considering risk tolerability – or what constitutes acceptable risk. We can also use stakeholder input – that's a very important consideration that underlies decisions made within the framework.
What is the value of this framework for blood operators?
It’s not just the structured approach. There's a strong element of stakeholder participation in the framework to inform decision-making, to conduct risk communication and to build trust. There's also a piece of the framework that focuses on health economics and analysis. So, taking a system view, we can determine where the risk resides and how to best allocate resources to it looking at that entire system, and looking at opportunity cost.
What sorts of decisions have been made using the framework?
We have completed a risk-based decision-making or "RBDM analysis" on Babesia risk in Canada, which informed the executive management team’s decision on Canadian Blood Services’ policy. We also have an analysis underway on CMV testing and we are conducting a risk-based decision-making analysis to inform our plasma strategy.
The framework is also being used internationally. Ireland has done an analysis on HTLV (Human T-lymphotropic virus), as has Australia. The U.K. has done work on pathogen inactivation regarding bacterial risk in platelets. And, we are also working with AABB to focus on analyses for both babesia and Zika.
(In the video below, Judie Leach Bennett describes the step-by-step process of the risk-based decision-making framework.)
Next: Making decisions the right way – a global endeavour – Part 2: RBDM analysis on Babesia in Canada
Canadian Blood Services – Driving world-class innovation
Through discovery, development and applied research, Canadian Blood Services drives world-class innovation in blood transfusion, cellular therapy and transplantation—bringing clarity and insight to an increasingly complex healthcare future. Our dedicated research team and extended network of partners engage in exploratory and applied research to create new knowledge, inform and enhance best practices, contribute to the development of new services and technologies, and build capacity through training and collaboration.
The opinions reflected in this post are those of the author and do not necessarily reflect the opinions of Canadian Blood Services nor do they reflect the views of Health Canada or any other funding agency.
Related blog posts
Dr. Sheila O’Brien knows the answer. She is the associate director, epidemiology and surveillance, working at Canadian Blood Services head office in Ottawa. Understanding and minimizing the infectious risks associated with blood transfusion is what she does each and every day.
A new innovation by a team of Canadian Blood Services researchers and the National HLA Advisory Committee has improved the situation for Canadian transplant patients. Launched in April 2012, the Canadian cPRA Calculator was developed to support Canadian Blood Services’ transplant programs. It’s a...