Estimating HIV risk
|
Project lead |
Trevor Hart (Toronto Metropolitan University) |
|
Project team |
Greta Bauer (Western University); David Brennan (University of Toronto); Joseph Cox (McGill University); Daniel Grace (University of Toronto); Nathan Lachowsky (University of Victoria); Gilles Lambert (Montréal University); Sharmistha Mishra (St. Michael’s Hospital); David Moore (University of British Columbia); Darrell Tan (St. Michael’s Hospital); Shayna Skakoon-Sparling (Ryerson University) |
|
Partners and collaborators |
Joshua Edward (Nova Scotia Health, Dartmouth); Dane Griffiths (Ontario Gay Men’s Sexual Health Alliance, Toronto); Jody Jollimore (CATIE,); Maya Kesler (University of Toronto); Syed Noor (Louisiana State University in Shreveport, Shreveport); Greg Oudman (Health Initiative for Men, Vancouver); Frédérick Pronovost (RÉZO Montreal); Roustam Souleymanov (University of Manitoba, Manitoba) |
|
Timeline |
Oct 2017 – Mar 2022 |
|
Funding |
$452,500 |
|
This summary was written by the project team with support from a Canadian Blood Services' knowledge broker. Last Updated: February 2024 Disclaimer: This research project is funded through the MSM Research Program. The objective of the MSM Research Program is to ensure the generation of adequate evidence-based research for alternative screening approaches for blood or plasma donors, which could evolve the current deferral policy for men who have sex with men while maintaining the safety of the blood supply. The Program is administered by Canadian Blood Services and Héma-Québec with funding support from the Federal Government (Health Canada). The views herein do not necessarily reflect the views of Canadian Blood Services, Héma-Québec, or the federal, provincial, or territorial governments of Canada. |
|
Project Summary
Background
Mathematical modelling of potential risks of any changes to the eligibility criteria for men who have sex with men (GBM) to give blood and plasma is needed, both in the current blood safety context and if alternative risk reduction strategies (e.g., pathogen reduction technologies) are applied in the future. This project aims to generate new data and better risk forecasting to help guide Canadian blood donor policies. Using data from HIV-negative gay and bisexual men living in Montreal, Toronto, and Vancouver, this study estimated the incidence of HIV among a representative sample of GBM. Participants were asked about their understanding and acceptance of different, personal questions about their sexual history that could be used to screen out donors who are likely to be HIV-positive, as well as the likelihood of donating blood under alternative screening policies.
What was done?
This project is a 1-year follow-up of HIV-negative participants already recruited through a cross-sectional study called The Engage Study. Engage is a mixed-method cohort study being conducted in Vancouver, Toronto, and Montreal. Engage recruited cisgender and transgender men who were at least 16 years of age at baseline and reported having sex with another man in the past six months. The baseline sample was recruited using respondent driven sampling.
At Engage study visits, participants complete computer-assisted surveys (in French or English) and biomedical testing. These tests include STI testing for Gonorrhea, Chlamydia, Hepatitis B & C, and Syphilis, as well as HIV testing. At 1-year follow-up visits (May 2018 – Feb 2021) participants repeat the baseline self-report questionnaire, with items added related to the comprehension and acceptability of current and alternative behaviour-based blood donor screening questions. Participants also undergo the same biomedical testing as at baseline.
The baseline sample for the Engage study includes 1,982 lab-confirmed HIV-negative men, and we have now completed 1-year follow-up visits with 1,297 HIV-negative/unknown participants (725 in Montreal, 237 in Toronto, and 350 in Vancouver). The average age of the baseline sample of 34.9 years (SD = 12.2, median = 31), and the majority identify as gay (81%), bisexual (7%), or queer (8%). Using participant data from study visits that were conducted between February 2017 and August 2021 among participants who were HIV-negative at baseline (n= 2008), we estimated rate ratios for HIV infection and the predictive ability of blood donation eligibility criteria to detect seroconversion. We used RDS-adjusted Poisson regression.
What was found?
Across all three cities, the HIV incidence rate was 0.4|100 person-years [95%CI: 0.3, 0.6]. The following factors were associated with HIV seroconversion in our sample: being under 30 years of age (adjusted rate ratio [aRR]= 9.1, 95%CI: 3.2, 26.2), reporting between 6 and 10 sexual partners in the past six months (aRR= 5.3, 95%CI: 2.1, 13.5) or over 10 sexual partners in the past six months (aRR= 8.4, 95%CI: 3.4, 20.9) (versus reporting 1-6 sexual partners), and reporting the use of crystal methamphetamine during sex in the past six months (aRR= 4.2, 95%CI: 1.5, 11.6). It was determined that the following selection criteria would result in 100% sensitivity (and 100% negative predictive value) for detecting Engage participants who seroconverted: use of injection drugs, > 2 anal sex partners, and any new anal sex partners. Such selection criteria would also result in deferring 63% of Engage study participants from donating.
Regarding attitudes towards blood donation eligibility questions, only a minority of men reported that they would be willing to donate blood under a time-based MSM deferral policy, regardless of the time span specified. However, the majority of MSM would comply with either a 3- 6- or 12-month deferral (i.e., would not attempt to donate blood) – although only a minority found time (vs. behaviourally) based policies to be acceptable.
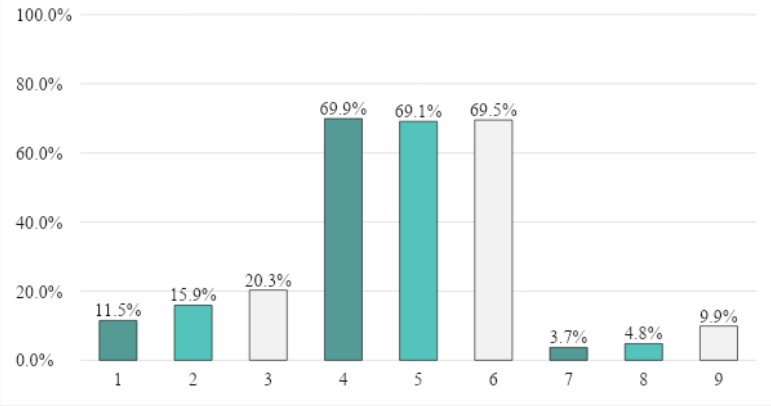
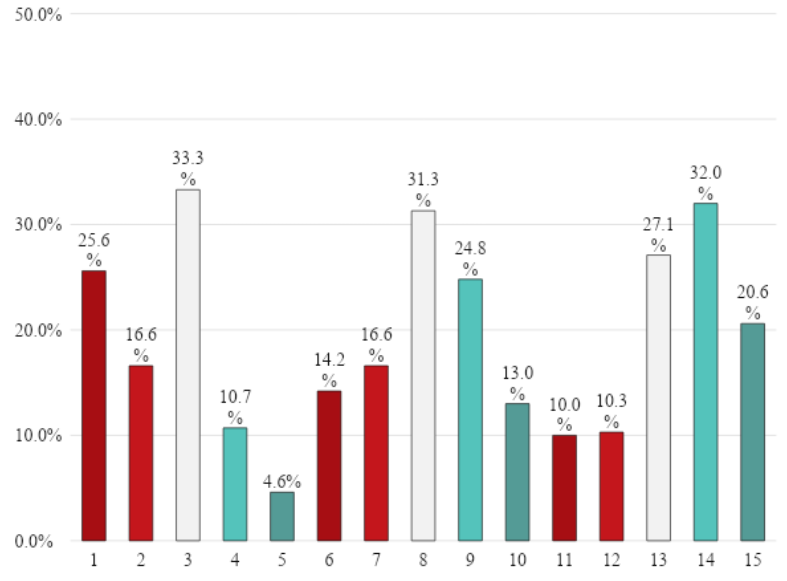
These findings suggest that the vast majority of MSM do not find time-based deferral policies to be acceptable, including the recent change to a 3-month deferral policy. There were mixed findings on other alternative policies, such as allowing HIV-negative MSM who use PrEP to be eligible to donate blood. The present findings do not suggest that the new 3-month deferral policy would lead to increased interest among MSM to donate blood.
Further, our findings suggest that using three behaviourally based questions regarding substance use and sexual partners in the past 6 months would correctly identify potential donors (including GBM donors) who could be considered at elevated risk for having recently contracted HIV. Moving to these questions would also reduce the proportion of sexually active GBM who are deferred from blood donation by one-third, thus potentially increasing the number of potential blood donors among GBM.
Opportunities for change
Despite adjustment using RDS-II weights, some GBM could still be under-or overrepresented. Since recruitment was limited to the three largest cities in Canada, results may not be generalizable to GBM living outside large urban areas. However, the HIV epidemics in each province are highly concentrated among GBM living in these cities.
The proportion of participants that were lost to follow up (LTFU) after baseline, having no follow-up visits, was 16%, 29% and 22% in Montreal, Toronto and Vancouver, respectively. Covariate imbalance between LTFU and non-LTFU participants was small (SMD values between 0.1 and 0.3146) and limited to the following HIV predictors: chemsex, sex with HIV-positive partners, age under 30 years and injection drug use. As such, it is unlikely that LTFU affected negative predictive values estimates.
Blood operators are concerned by HIV infections acquired in the 3 months preceding a blood donation, whereas Engage provides information on participants' behaviors in the 6 months preceding study visits. Due to missed visits, three participants were diagnosed with HIV more than 1 year after their last study visit. Behaviors reported then were assumed to reflect behaviors at the time of infection.
Future considerations
Future mathematical models of HIV transmission will examine how to partition the MSM population such that one or more groups would have a risk estimate for incident HIV infection comparable to that of current non-deferred groups. This will help inform a safer and more equitable blood donation policy in Canada.Research publications
Research publications and resources
Lambert, G., Cox, J., Fourmigue, A., Dvorakova, M., Apelian, H., Moodie, E. E. M., Grace, D., Skakoon-Sparling, S., Moore, D. M., Lachowsky, N., Jollimore, J., Lal, A., Parlette, A., Hart, T. A., & Engage Study Team (2022). HIV incidence and related risks among gay, bisexual, and other men who have sex with men in Montreal, Toronto, and Vancouver: Informing blood donor selection criteria in Canada. Transfusion, 62(12), 2555–2567. https://doi.org/10.1111/trf.17127
Hart, T. A., Moore, D. M., Noor, S. W., Lachowsky, N., Grace, D., Cox, J., Skakoon-Sparling, S., Jollimore, J., Parlette, A., Lal, A., Apelian, H., Sang, J. M., Tan, D. H. S., Lambert, G., & Engage Study Team (2021). Prevalence of HIV and sexually transmitted and blood-borne infections, and related preventive and risk behaviours, among gay, bisexual and other men who have sex with men in Montreal, Toronto and Vancouver: results from the Engage Study. Canadian journal of public health = Revue canadienne de sante publique, 112(6), 1020–1029. https://doi.org/10.17269/s41997-021-00546-z
Knowledge-to-Action
Findings from this research provided support that the sexual behaviour-based screening questions, in addition to other deferral criteria that will remain in place, will maintain safety.