MSM Research Program
Knowledge Synthesis Interim Report
March 2020
In brief
Canadian Blood Services and Héma-Québec are responsible for ensuring the safety and sufficiency of the national blood supply. Both organizations are committed to advancing Canada’s blood system. They continue to lead activities to advance the donor eligibility criteria specific to men who have sex with men (MSM). Through the MSM Research Program, a unique and focused national effort to create scientific knowledge, Canadian blood operators are supporting 15 research projects to generate evidence necessary to advance MSM blood donor criteria.
At an MSM Knowledge Synthesis Forum (the ‘Forum’) held on Nov. 6–7, 2019, the research teams presented their preliminary results and engaged in open dialogue with attendees on what these findings mean and their potential impact. The Forum was hosted by Canadian Blood Services and Héma-Québec. Forum attendees included representatives from several international blood operators and organizations, Health Canada, the Public Health Agency of Canada, LGBTQ+ communities and patient organizations. This interim report provides an overview of the preliminary results and the discussions that took place.
Three broad principles were considered during discussions on the preliminary findings: acceptability, safety and feasibility.
Discussions at the Forum highlighted an appreciation of the volume of data generated so far, the dedication of the research teams and the stakeholders, and the commitment of Canadian blood operators. The need for better knowledge dissemination from blood operators regarding blood donor eligibility criteria and the evidence supporting the criteria was raised. Ongoing research is needed to continue to build the evidence base to advance Canada’s blood donor policy for MSM.
Explore the report sections
Advancing donor eligibility
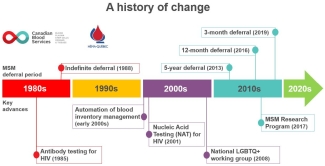
At the start of the Forum, participants were given an overview of the process to change blood donor eligibility criteria, and a history of changes to blood donor eligibility for MSM in Canada.
Canadian Blood Services and Héma-Québec, the two blood operators in Canada, are responsible for providing safe blood components and blood products and for ensuring their supplies meet patient needs. In Canada, blood and blood components intended for transfusion or for further manufacture into drugs for human use are regulated. Health Canada is the blood system regulator. Health Canada regulations are in place to protect patients and the sufficiency of the national blood supply. Included in the regulations are requirements related to blood donor eligibility criteria, which are part of a multi-level safety system to protect the blood supply.
Process for change
Blood operators must apply to Health Canada for approval before they can make changes to donor eligibility criteria. The application must justify the proposed change and present enough evidence to show that the change will not bring increased risk to the safety or the sufficiency of the blood supply. Evidence is largely based on data gathered from research, surveillance studies, and stakeholder engagement.
MSM blood donor eligibility
Every blood donor undergoes screening before each donation to ensure they are eligible to give based on current blood donor criteria. An important part of this screening is the donor health questionnaire. This extensive list of questions asks about the donor’s health and their potential exposure to transfusion-transmissible infectious diseases.
In Canada, MSM were first indefinitely deferred from blood donation in 1988 when they were noted to be a particularly high-risk population for HIV/AIDS. For over 10 years, Canadian blood operators have been on a journey to advance donor eligibility for MSM using an evidence-based, step-by-step approach.
Currently, men who want to donate blood in Canada are asked if in the last three months they have had sex with a man. As of June 2019, men are eligible to donate blood if it has been more than three months since their last sexual contact with a man.
This population-based risk approach to blood donor screening is viewed by many as discriminatory and changing this approach as an issue of social justice. Improvements in testing technologies, inventory management, and the accumulation of scientific evidence has supported the incremental advancement in donor eligibility criteria for MSM. These changes have occurred within an evolving social and political landscape. Further advances to MSM donor eligibility criteria require a body of evidence that shows that proposed changes will not negatively impact the safety and sufficiency of the blood supply.
The objective of the MSM Research Program is to ensure the generation of adequate evidence-based research for alternative screening approaches for blood or plasma donors, which could evolve the current deferral policy for men who have sex with men (MSM) while maintaining the safety of the blood supply.
Generating knowledge
Following a stakeholder meeting in January 2017 to identify research priorities, Canadian Blood Services and Héma-Québec launched the MSM Research Program (the ‘Program’). This unique Program funds 15 innovative research projects to generate evidence that is currently lacking. Canada is the only country undertaking such a focused program. It is guided by a knowledge mobilization strategy that prioritizes stakeholder engagement, communication of research results, and effective synthesis of these results. The results will inform advances in MSM eligibility criteria in Canada and may help guide advances in other countries.
Many projects supported by the Program are ongoing, with most results expected in 2020 and 2021. To begin the process of integrating any early findings from the research projects, a Knowledge Synthesis Forum (the ‘Forum’) was held in Toronto in November 2019. Researchers funded by the Program presented their results so far. Other participants included Canadian and international experts (U.S.A., U.K., France and Australia), LGBTQ+ communities and patient organizations, and representatives from Health Canada and the Public Health Agency of Canada.
All attendees were provided information about the research projects ahead of the Forum to enable them to participate actively in discussions during the event. The following section outlines the research progress presented and the highlights of the discussions that took place at the Forum.

According to post-event survey results, 82 per cent of participants agreed the Forum successfully met its objectives to:
- Inform/update participants on the state of the field internationally since the 2017 meeting “Next steps for the MSM donor policy: Setting the research agenda”
- Facilitate the transfer of knowledge generated thus far by the MSM Research Program
- Begin the process of synthesizing the knowledge generated thus far by the MSM Research Program with dual objectives:
1) Identify any remaining and emerging knowledge gaps, and
2) Determine how the knowledge generated can be applied to inform the evolution of the MSM donor eligibility criteria for blood donation.
Synthesizing the evidence
Project updates
Sessions at the Forum reflected the Program’s research priorities. Each project addresses one or more of these priorities and three or four projects were presented in each session.
Developing alternative eligibility criteria
Results suggest many gbMSM support changing the blood donor eligibility criteria. A high percentage of gbMSM would be willing to donate blood if they were eligible to do so. Research is underway regarding issues of privacy, confidentiality and access to blood donation for gbMSM living in rural and urban areas. Research is also underway to understand the experiences of blood donation specific to diverse gbMSM communities, such as those who identify as African, Caribbean and Black. The importance of relationship repair with communities affected by MSM-related donor policies arose from research presented in this session and the next, and in discussions at the Forum.
Acceptability of alternative policies
The current approach to MSM donor eligibility considers MSM as a population and assesses transfusion-transmissible infectious disease risk in that population as a whole rather than assessing risk based on an individual’s behaviour. The majority of gbMSM surveyed view the current population-based risk approach as discriminatory and therefore not acceptable. Findings of research conducted to date suggests that the order in which questions are currently asked in the donor health questionnaire (i.e. proximity of the MSM question to socially stigmatized behaviours) may unintentionally generate negative implicit bias toward gbMSM in people completing the questionnaire. Among gbMSM study participants, there was limited understanding of, or excitement for, an MSM plasma donation program where the donated plasma would be used to manufacture plasma protein products (i.e. drugs) to treat patients. Research is examining whether changing to an individual behaviour-based approach to donor screening (vs. the current population-based approach) would be acceptable, and how it would impact current donors’ intentions to donate and donor deferral rates.
Risk modelling
Risk modelling is used to assess how changes to donor eligibility criteria might impact blood safety and sufficiency. Risk modelling research funded by the Program suggested that the additional risk with a three-month MSM deferral period would be very low. These results informed an application to Health Canada to make this change in 2019. Research is examining the prevalence and incident rates of HIV in a gbMSM population identified as low-risk based on sexual behaviour. Several potential behavioural indicators that could be used in an individual behaviour-based donor screening process are also being studied.
Operational feasibility
The operational feasibility of screening all donors using individual risk-based questions (e.g. asking about number of sexual partners, or number of new partners, or sexual behaviours) was investigated. Preliminary results suggest that applying an individual risk-based screening approach to all whole blood donors may increase deferrals, particularly in younger age groups. This could result in a significant loss of currently safe donors. Other studies are addressing the feasibility of a plasma donation program for MSM. While gbMSM study participants expressed some interest in such a program, barriers exist. These include a lack of knowledge about plasma donation, the stigma associated with applying any differential treatment to MSM plasma donations, and an ongoing inability for sexually active gbMSM to donate whole blood.
Applying the research knowledge
Three broad principles were considered during discussions about the preliminary research findings: acceptability, safety and feasibility. These principles can be applied to the various approaches that are addressed by the research (e.g. the current population-based approach with time-based deferrals; applying an individual risk behaviour-based approach to all donors or to MSM for either whole blood donation or plasma donation).
Acceptability
- Even if the current population-based risk approach led to a shorter time-based deferral period, it would likely not yield many more donors and does not address the perception that the policy is discriminatory.
- There was much discussion about use of a “capture” question, which is a screening question to identify MSM donors and direct them to additional questions that assess risk behaviours. It is not clear if this would be acceptable to gbMSM, even if it was viewed as a stepping stone towards more inclusive criteria and may result in eligibility of a cohort of gbMSM with behaviors associated with a lower risk of infectious disease exposure.
- The most acceptable approaches are those that are viewed as equitable (i.e. apply the same screening to everyone).
- Donors (and Canadians in general) need to understand the reason behind screening questions and deferrals (not only those related to MSM). Whatever approach to donor policy is taken, there is a clear need for coordinated education and communication to ensure current and prospective donors, patients and patient groups understand the blood donor eligibility criteria and the evidence supporting them.
Safety
- Risk modelling research informed the Health Canada application requesting a change to a three-month deferral period for men since their last sexual contact with a man.
- The consensus from experts at the Forum was that once the ongoing studies are completed, we will have better data to inform risk modelling studies and potential future changes to the eligibility criteria.
- While some potential ways to screen donors based on behaviours associated with higher infectious disease risk were discussed (e.g. number of sexual partners), more research is needed to identify which indicators would be most effective, acceptable, and feasible.
Feasibility
- When considering asking risk behaviour-based questions for all donors, the impact on the number of currently eligible donors must be considered. Too great a loss of current donors may affect the sufficiency of the Canadian blood supply.
- For any approach to be successful, clear communication of why donors are being asked screening questions is essential, particularly if those questions might make people uncomfortable and discourage them from donating.
- If potential donors are being asked to provide sensitive or potentially stigmatizing information, privacy/confidentiality would need to be assured. The risk of stigmatization could be a barrier to donation for some MSM.
- There was some interest among gbMSM study participants in a plasma donation program where donations would be used to make plasma protein products to treat patients. However, there are also potential barriers. More education about plasma donation is needed. Two research projects are underway to examine the feasibility of this kind of program.
Emerging challenges in blood donor eligibility criteria
Pre-exposure Prophylaxis (PrEP) and Post-exposure Prophylaxis (PEP)
Currently, Health Canada requires the blood operators to defer donors taking PrEP/PEP. PrEP/PEP may delay the time from infection to detection and interfere with infectious disease testing of donated blood. This area requires further research.
U ≠ U for blood transfusion
U = U, or “Undetectable equals Untransmittable”, is a global informational campaign about how effective HIV medications are in preventing sexual transmission of HIV. It is based on evidence that the risk of sexual transmission of HIV is zero if viral load is low (<200 copies/ml). However, this campaign does not apply for blood transfusion. This is because during transfusion a large volume of blood is delivered intravenously, that is, directly into the blood stream. In this way, even a very small number of viral particles could transmit the infection. While blood operators test every donation for HIV, the sensitivity of the testing method may not be enough to detect low viral loads. It is thus important that the public understand the potential risk to the blood system and the need to disclose their HIV status as well as refrain from blood donation.
Trans blood donors
There is a lack of data and research on blood donor policy specific to trans and gender non-binary individuals. Although research on trans blood donation is specifically not addressed by the Program, the impact MSM eligibility criteria has on trans communities came up frequently, highlighting this as an area that needs more research and attention by the blood operators.
According to post-event survey results, 96 per cent of participants agreed the Forum provided opportunities to engage in the discussion.
Knowledge Café
During the “Knowledge Café”, Forum participants were split into three groups. In these groups, they had facilitated discussions focused on three broad questions ("What have we learned?", "What does it mean?" and "How to share what we've learned?"). Forum participants’ responses to the questions were captured and collated. Below are some of the Forum participants’ opinions as expressed during the Knowledge Café.
What research did you find most compelling or most important?
Participants:
- Appreciated the sheer volume of data generated, the dedication of the research teams, and the commitment from Canadian Blood Services and Héma-Québec to advance blood donor eligibility criteria specific to MSM.
- Recognized the challenge of developing more inclusive eligibility criteria while protecting blood safety and sufficiency.
- Found very compelling the study that indicated that the order of questions in the donor health questionnaire could lead to implicit bias.
- Found important the studies that suggested relationship repair with affected communities will be needed.
- Felt that being inclusive, bringing marginalized voices to the centre; and including trans perspectives, and ethnically diverse/multicultural perspectives are necessary to effectively advance blood donor policy.
What research or information gaps did you notice?
Participants noted:
- A lack of data about:
- Trans donors;
- African, Caribbean and Black (ACB) and other marginalized groups within LGBTQ+ communities.
- Research gaps remain around:
- The impacts of further evolving the criteria (e.g. who will start or stop donating blood if criteria are changed);
- How new technologies and innovation (including pathogen reduction technologies) might impact the basis of donor eligibility criteria;
- How best to identify sexually active low-risk MSM;
- Which questions might be used to apply a gender-blind or individual risk-behaviour-based screen to all donors;
- Trans donor screening.
- There is a need for:
- Better education, particularly of deferred donors to help them understand why they are deferred;
- More effective engagement, particularly with marginalized groups including trans and ACB gbMSM communities;
- Clearer explanations of the scientific basis of current and future blood donor eligibility criteria.
How do you think this current research might affect you/your community?
Participant responses:
- Patient groups recognized the current eligibility criteria are viewed as discriminatory and understood social justice concerns raised by current donor eligibility criteria. They believe that the evidence being gathered will assure them of the continued safety and sufficiency of the blood supply.
- Echoing the research findings, several participants felt there was a need for relationship repair with communities historically affected by the criteria, in particular marginalized groups such as ACB gbMSM.
- Some felt that blood operators have a responsibility to affected communities and need to think carefully about how to best position alternative approaches to blood donation by MSM (e.g., a plasma donation program for MSM, MSM “capture” question).
Based on current findings, what actions or next steps would you suggest to Canadian Blood Services and Héma-Québec to readily move towards broader eligibility criteria?
Participants suggested:
- Re-ordering or repositioning of screening questions to reduce implicit negative bias towards gbMSM.
- Blood operators need to improve and modernize their communication, social marketing and education; information should be easier to access than it currently is. Better communication and education could help improve relationships with affected communities.
- The regulators and blood operators need to be more transparent about what evidence is required to make further changes.
How would you/your community share and make use of the knowledge generated by the Program?
Participants said:
- That knowledge dissemination should be specific to the audience, well-timed, with a clear aim. Follow through with change to the eligibility criteria is critical.
- Audiences for knowledge dissemination should include blood operator staff (to help build confidence among people who receive and donate blood) and the next generation of researchers, health-care providers / clinical practitioners; students, as well as LGBTQ+ and patient groups.
- More information about the rationales for donor deferrals is needed for the general public.
- Knowledge dissemination and communication from a social-equity lens (i.e. for whom-by whom?) needs to be considered; inclusion and participation of diverse community groups throughout knowledge dissemination processes is important.
How can Canadian Blood Services and Héma-Québec best disseminate the research findings?
Participants said:
- An anti-stigmatizing, anti-discriminatory perspective should be applied to communications.
- Consider safety and how to avoid stigmatizing communities/marginalized groups.
- Be aware that not all research will speak to all groups (e.g. ACB gbMSM, trans communities); apply an intersectional approach when considering communication with diverse groups.
- Work with community groups (e.g. co-create materials to ensure communities’ values and perspectives are acknowledged) but recognize the burden of effective communication lies with the blood operators, not the communities.
- Traditional written reports may not be the most effective way to disseminate this knowledge effectively to all audiences. Multimedia, social media, videos, webinars, etc., should be considered.
Next steps
Most research projects are still ongoing. Further collaboration and knowledge dissemination can be expected when the projects have been completed.
The blood operators:
- Will ensure what was learned and heard at the Forum is disseminated internally at the blood operators to increase awareness of research evidence and challenges, and to inform change;
- As the research projects conclude over the next two years, will commit to continuing the process of knowledge synthesis and dissemination of the research results;
- Will continue good-faith engagement with stakeholders toward more inclusive blood donor eligibility criteria in Canada;
- Will develop educational materials to equip donors, the public and blood operators’ staff with information about blood donor eligibility criteria and deferrals;
- Will continue working toward improving donor screening, including revisiting the placement of MSM-related questions in the donor health questionnaire to avoid the creation of unintentional bias against gbMSM resulting from the screening process.
Interested in learning more?
If you'd like to learn more about the research funded under the MSM Research Program? Please contact the Canadian Blood Services’ Centre for Innovation by e-mailing: centreforinnovation@blood.ca
Acknowledgements
The Knowledge Synthesis Forum was organized by Canadian Blood Services and Héma-Québec who developed and continue to manage the MSM Research Program. Funding for the MSM Research Program was provided by Health Canada. The views herein do not necessarily reflect the views of Canadian Blood Services, Héma-Québec, or the federal government of Canada.
Canadian Blood Services and Héma-Québec are sincerely grateful to the research community and the participants at the 2019 Knowledge Synthesis Forum for their engaged and passionate input, and to the many individuals and stakeholder groups that have been actively involved in efforts to advance the MSM donor policy over more than a decade. This report contains only the highlights of the 2019 Forum. We would like to assure Forum participants that further details of the Forum presentations and discussions were captured and are being incorporated into internal processes to drive advancement by the blood operators.
Footnotes
Report prepared by: Geraldine Walsh, Jennie Haw and Sophie Chargé, Centre for Innovation, Canadian Blood Services, in consultation with the MSM Research Program Planning Committee: Chris Brennan, Gilles Delage, Dana Devine, Marc Germain, Mindy Goldman, Don Lapierre, Sheila O’Brien & Adrienne Silver
A note regarding terminology in the report: “MSM” encompasses all men who have sex with men however they identify and is used as a proper noun when referring to specific criteria and programs (e.g. MSM eligibility criteria or MSM Research Program). The acronym “ gbMSM ” for gay, bisexual and other men who have sex with men, is used when referring specifically to these communities.
MSM Research Program priorities include: Research to inform the development of an individual risk assessment donor policy (behavioural based) or to strengthen the existing policy (population based); Research to evaluate operational feasibility of alternative donor deferral policies and their acceptability by Canadians; Risk modeling and surveillance to assess the risk associated with alternative donor selection policies; Research to evaluate the impact of alternative risk reduction
technologies on donor screening.
Additional resources
About the blood operators
About the stakeholder organizations that participated in the forum*
- Canadian Hemophilia Society
- Community-Based Research Centre
- Immunodeficiency Canada
- Pride London Festival
- Sickle Cell Disease Association of Canada
- Thalassemia Foundation of Canada
*The following organizations were invited to the Forum but were unable to attend: Canadian Immunodeficiencies Patient Organization, COCQ-SIDA, and Canadian Centre for Diversity and Inclusion.
About the MSM Research Program
- Research Program project descriptions
- MSM Research Program information
- 2017 International meeting
- Funding round 2
- Blog post 1
- Blog post 2
Links to MSM Research Program published papers
- Goldman et al., 2018: Donor deferral policies for men who have sex with men: past, present and future (article available free online)
- Caruso et al., 2019: 'One step closer': Acceptability of a programme of plasma donation for fractionation from men who have sex with men (article available free online)
- Davison et al., 2019: Changing the deferral for men who have sex with men - an improved model to estimate HIV residual risk
- Grace et al., 2019: Gay and Bisexual Men's Views on Reforming Blood Donation Policy in Canada: A Qualitative Study (article available free online)
- O’Brien et al., 2019: HIV residual risk in Canada under a three-month deferral for men who have sex with men
Further reading
- Blog post: The things we do for safety: Leukoreduction
- Book chapter: Donor Selection, Donor Testing and Pathogen Reduction
- Canadian Blood Services’ Surveillance report 2021