Improving patient safety: preventing a harmful side effect of IVIg treatment
Friday, April 09, 2021 Guest Author
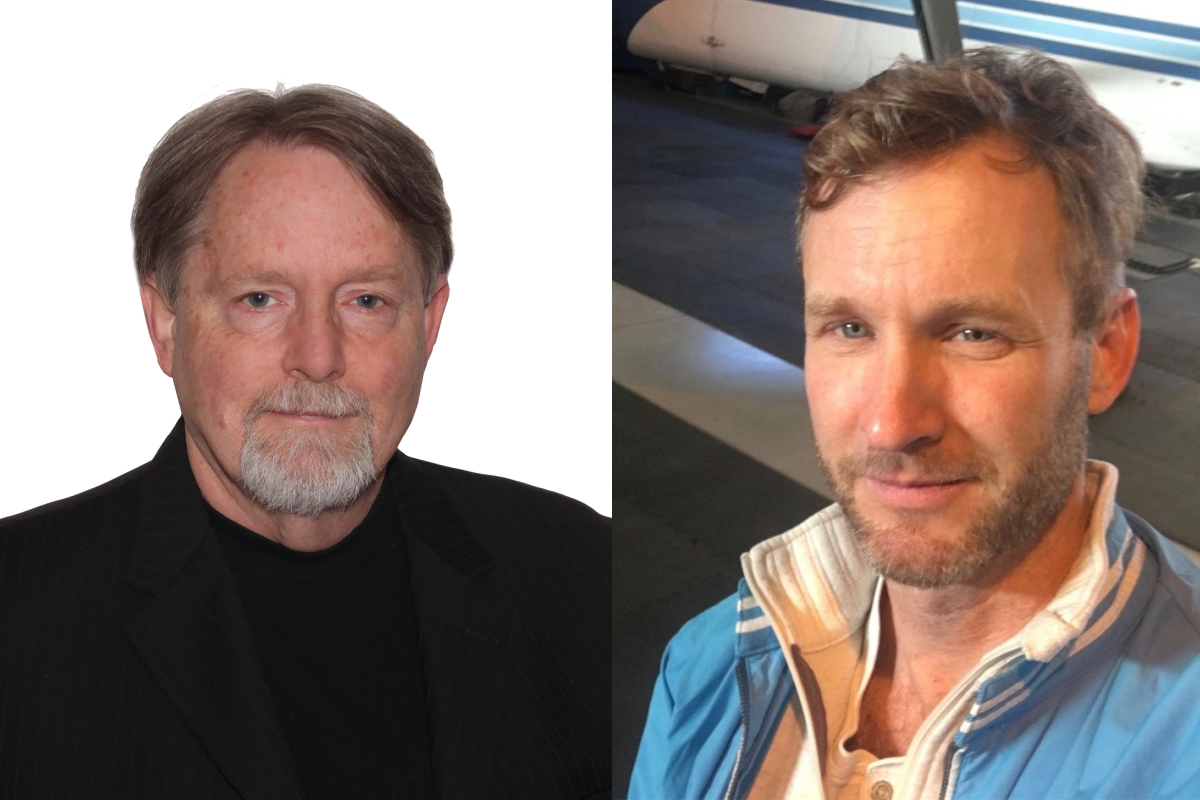
By Dr. Donald Branch and Dr. Jacob Pendergrast
Dr. Donald Branch is Senior Scientist, Canadian Blood Services Centre for Innovation, and Professor in Medicine at the University of Toronto. Dr. Jacob Pendergrast is Associate Medical Director, Blood Transfusion Laboratory, University Health Network, and Assistant Professor, Department of Laboratory Medicine and Pathobiology at the University of Toronto.
Research conducted by our team at the University of Toronto QUEST program and supported by Canadian Blood Services is improving patient safety for those who need intravenous immune globulin (IVIg), a drug used to treat autoimmune diseases. By increasing our understanding of an unexpected, potentially life-threatening side effect of IVIg therapy, our studies can help doctors better predict which patients are most at risk and take steps to protect them.
An unexpected side effect
Made of antibodies from the plasma of tens of thousands of human donors, IVIg is a purified blood product used to suppress abnormal or unwanted immune responses. It’s used to treat patients with a variety of conditions, including immune thrombocytopenia (ITP) and Guillain-Barré Syndrome (GBS). Because it’s so effective in treating conditions for which substitute treatments are not yet available, use of IVIg has increased dramatically. But with this increased use came reports of an unexpected side effect: some patients treated with IVIg were experiencing hemolysis, the rapid destruction of their red blood cells. Although most cases of hemolysis are mild, some cases can be severe and require red blood cell transfusion and/or other methods of life-support.
Who’s at risk
Hemolysis appears to involve antibodies naturally occurring in the donor plasma used to make IVIg. These antibodies are called ABO antibodies or ABO isoagglutinins. Our research team wanted to further investigate IVIg-associated hemolysis: how often does it happen, how can diagnosis be improved, and why does it happen to some patients but not others.
Through a number of published research studies, we were successful in answering these questions.
- In our study published in the journal Transfusion we reported that the incidence of hemolysis following IVIg therapy is common—higher than previously thought—and frequently severe.
- In a letter to the editor in the journal Blood, we reported that blood group genotype (referred to as ABO zygosity) was the main risk factor for IVIg-associated hemolysis. We showed that blood group AB people are at highest risk, heterozygous AO or BO are at lowest risk, while group O people are not at risk.
- In the same Transfusion study, we learned more about the ABO antibodies associated with patients’ red blood cells: they were of the subclass IgG2. Knowing this provides valuable insights into the immune response and mechanism of hemolysis.
- A paper published in Transfusion showed that a test called a phagocytosis assay could help in diagnosing IVIg-associated hemolysis.
Preventing or minimizing hemolysis
Our research led us to propose two key things that can be done to improve patient safety: (1) People with blood group AB who receive IVIg should be closely monitored for hemolysis and (2) Reduce levels of ABO antibodies in IVIg. These findings are relevant to doctors who prescribe IVIg to their patients and to scientists trying to better understand IVIg-associated hemolysis. Although the research suggests that the best way to minimize the risk of IVIg-associated hemolysis is to avoid IVIG therapy in people with blood group AB, or with the blood group genotype AA or BB, it’s just not a practical approach—there is a lack of effective IVIg substitutes and genotyping every patient is not routinely done. But the insights gained from our research move us closer to the goal of avoiding IVIg-associated hemolysis altogether.
***
For more on this topic, watch the presentation, Exploring the frontiers of IVIg-associated hemolysis, given by Drs. Pendergrast and Branch.
Canadian Blood Services – Driving world-class innovation
Through discovery, development and applied research, Canadian Blood Services drives world-class innovation in blood transfusion, cellular therapy and transplantation—bringing clarity and insight to an increasingly complex healthcare future. Our dedicated research team and extended network of partners engage in exploratory and applied research to create new knowledge, inform and enhance best practices, contribute to the development of new services and technologies, and build capacity through training and collaboration. Find out more about our research impact.
The opinions reflected in this post are those of the author and do not necessarily reflect the opinions of Canadian Blood Services nor do they reflect the views of Health Canada or any other funding agency.
Related blog posts
With an anticipated global shortage of immune globulin products, finding alternatives to IVIg can help improve availability of a drug in high demand. A recent study shows that eltrombopag, an oral medication that stimulates the production of platelets, is an effective alternative to IVIg for patients with immune thrombocytopenia who need surgery.
Blood plasma-derived IVIg holds promise as a treatment for Alzheimer’s disease. A new study suggests that combining IVIg with a new drug delivery technique that helps get IVIg into the brain could increase its effectiveness and help make the best use of this precious treatment.
A study conducted by researchers in the University of Toronto QUEST program, a research collaborative supported by Canadian Blood Services, looked at what can be done to reduce the number of inappropriate red blood cell transfusions in hospitals.


