This is why we need a diverse donor base

A patient’s life or health may depend on blood components, stem cells or even an organ from a donor of similar ethnic background
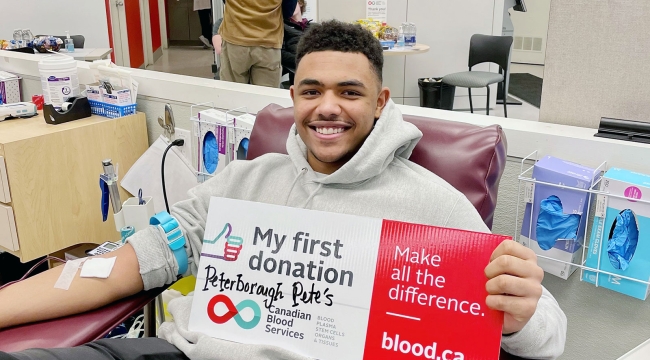
While one in every two people in Canada are eligible to donate blood, plasma or platelets, only one in 81 do. We need many more new donors — 100,000 each year — to keep Canada’s Lifeline strong.
People of all backgrounds can help. In fact, ethnic diversity is essential for saving lives. Perhaps you’ve already heard that a patient’s best hope of a lifesaving stem cell transplant may be a donor who shares their ethnic background (so please, join the stem cell registry if you’re aged 17 to 35 and in good health!). But did you know many patients also need specially matched blood?
We need a donor base as richly diverse as Canada to meet the need for blood components — red blood cells, platelets and plasma — as well as for stem cells, organs and tissues. Learn more about why, for all 5 areas.
1. Red blood cells and diversity

Markers on your red blood cells called “antigens” determine your blood type. For example, if you have both the “A” and “B” antigen and another called “Rh D,” your blood type is AB-positive. On the other hand, if you have none of these antigens, you are type O-negative (also known as the “universal donor” and critical in emergencies).
The different ABO blood types are inherited and vary in frequency in different parts of the world. But they are also just one part of the story. Your red blood cells actually contain hundreds of antigens.
“When it comes to red blood cell transfusion, some of the other antigens become important to consider,” explains Dr. Aditi Khandelwal, a physician with Canadian Blood Services’ Medical Laboratory & Stem Cell Services division.

Some patients, including those with serious illnesses, need red blood cells to be matched to a more expanded combination of antigens. Because antigens are inherited, those that are common in one ethnic group may be less common in another.
“To be able to find those matches, it is very important that we have a donor base that looks more like the recipients, so we can meet every patient’s needs,” says Dr. Khandelwal.
Matching can be crucial for people living with sickle cell disease. This inherited condition is most common in people of African, Middle Eastern and South Asian ancestry.
During sickle cell crisis, the normally pliable, round red blood cells become stiff and elongated, and can get stuck in small blood vessels. Without early and effective treatment — which may include matched red blood cell transfusion— people with sickle cell disease suffer severe pain, anemia, blood clots and other serious complications. Ongoing red blood cell transfusions are also an important therapy to prevent further complications of sickle cell disease.
People with other diseases such as thalassemia and myelodysplastic syndrome, a form of cancer, also require large quantities of matched blood.
2. Platelets and diversity

Platelets are the component of blood that helps with clotting. We collect platelets from blood donations when we separate the blood into its components. You can also donate platelets through a process that returns the other blood components to your body during donation.
Some patients need platelets that are specially matched to their own Human Platelet Antigens (HPA) and Human Leukocyte Antigens (HLA). The odds of finding a match are one in four among biological siblings, and one in 10,000 among random donors. Here, too, one is more likely to find a match in a person of similar ancestry.
Matched platelets are frequently needed to help patients with cancer. They also allow fetuses and newborns to survive life-threatening bleeding in the final stages of pregnancy and immediately after birth.
3. Plasma and diversity

Plasma is the straw-coloured component of blood that makes up most of its volume. We collect plasma from blood donations that have been separated into components. You can also donate plasma through a process that returns the other blood components to your body.
Plasma is used two ways: to make lifesaving medications, and for transfusions.
For patients who receive medications made from plasma — which are manufactured by pooling plasma from thousands of donors at a time — there is no need for blood type matching at all. Yet a large, diverse plasma donor base remains important. Demand for these medications is skyrocketing around the world, so we need donors of all backgrounds to help meet the needs of patients in Canada.
“It's important to the future of the blood system that blood, platelet and plasma donation be attractive and accessible,” Dr. Khandelwal says. “We want everyone to be excited to donate if possible.”
Did you know that some people who are not eligible to donate blood are eligible to donate plasma? That includes many who have travelled to or lived in parts of the world where medications to prevent malaria are recommended. The eligibility criteria are different because when medications are made from plasma, the malaria parasite is removed. Learn more about malaria and blood and plasma donation.
When patients receive plasma transfusions, the plasma doesn’t need to match many specific markers that vary with ethnicity, as may be required with transfusions of red blood cells and platelets. But the plasma does need to be compatible with the patient’s ABO blood type.
Some donors also have a special role in plasma transfusion. People with AB blood (positive or negative) are “universal donors” for plasma, just as people with O-negative blood are universal donors for red blood cells. Their plasma is crucial in emergencies where there’s no time to check the patient’s blood type.
(Don’t know your ABO blood type? We’ll be able to tell you after we’ve tested your first donation of blood, plasma or platelets.)
4. Stem cells and diversity

Stem cells, specifically blood stem cells, are immature cells that can develop into any blood cell present in the body. A stem cell transplant is a potentially lifesaving treatment for more than 80 diseases and disorders.
Stem cell donors and recipients are matched according to inherited markers called Human Leukocyte Antigens (HLA). Yet most people in need of a transplant won’t have a match in their own family. In those cases, the best hope is an unrelated donor of similar ethnic background.
If you’re between the ages of 17 and 35, you could become someone’s lifesaving match by joining Canadian Blood Services Stem Cell Registry. Currently, people who are Black, Indigenous, Asian, Hispanic or mixed-race make up only about a third of registrants.
Umbilical cord blood is another valuable source of stem cells for transplant. Expectant parents can register online to donate cord blood to Canadian Blood Services’ cord blood bank. Cord blood is collected from the placenta and umbilical cord after the baby’s birth.
Our cord blood bank needs donors of all backgrounds. But it’s also the case that in transplants using cord blood stem cells instead of stem cells from an adult donor, the match does not need to be as precise. For that reason, cord blood may help patients without a match on the stem cell registry.
5. Organs and tissues and diversity

The more people choose to register as organ donors, the more lives can be saved. Only a small percentage of people die in such a way as to make it possible for them to become organ donors, so it takes many registrants to meet the need.
And while donated organs are not matched based on race or ethnicity, it is important to have a diverse donor pool. Organ donors and recipients need to have compatible blood types and certain tissue markers in common, and similar ancestry boosts the likelihood of a match.
“Everybody has some way to give to Canada's Lifeline, be it blood products, tissues, stem cells, volunteering, financial donations, or working with their communities,” Dr. Khandelwal says. “That's where the real power of diversity lies.”
Ready to make all the difference? Explore all ways to give or book an appointment now to donate blood or plasma. Together, we are Canada’s Lifeline.