Thinking of joining the stem cell registry? Here’s what happens after you swab

We analyze the tiny sample of cells from inside your mouth for some specific genetic characteristics
Right now, hundreds of people in Canada are waiting for a stem cell transplant, a potentially lifesaving treatment that is only possible with a matching stem cell donor.
If you’ve already joined the stem cell registry, or are thinking about it, perhaps you’re curious about how we make those matches — including the role of your health information.
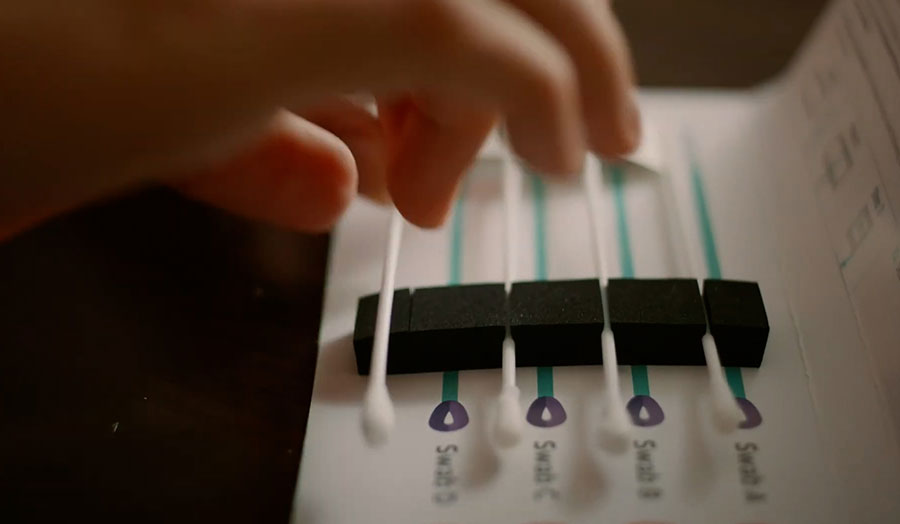
The registration process starts with what’s called a “buccal swab.” The registrant rubs the insides of their cheeks with the soft-tipped swabs in their free registration kit, to painlessly collect a small sample of their cells. Canadian Blood Services then analyzes the DNA from those cells for particular characteristics.
“We're not looking at the registrant’s whole gene map,” explains Dr. Matthew Seftel, a physician with Canadian Blood Services’ medical laboratory and stem cell services division. “We’re only looking at a very small number of genes that make up the code for the human leukocyte antigen system, or HLA.”
Analyzing the buccal swab for the registrant’s HLA characteristics involves a process called polymerase chain reaction, or PCR — the same technique used for detecting COVID-19 in small biological samples.
“The common theme there is that you need only a tiny amount of DNA to be able to analyze the HLA genes, in the same way that you only need a tiny bit of mucus from your nostril to be able to detect the genetic signature of the virus that causes COVID-19,” says Dr. Seftel.
The closer the HLA match between stem cell donor and recipient, the better. This helps to ensure the development of new, healthy blood cells in the recipient after the transplant. It also reduces the risk of a serious post-transplant complication called graft-versus-host disease, where cells from the donor see the patient’s cells as foreign and mount an attack.

As part of the registration process, the registrant gives consent for their HLA test results to be entered into the database for Canadian Blood Services Stem Cell Registry. No other tests are performed on the buccal swab samples, which are securely disposed of as biomedical waste in accordance with provincial and federal regulations.
The path to donating stem cells
Transplant centres search the stem cell registry database when seeking HLA matches for their patients. They see registrants identified by number only. If you’re matched to a patient, the transplant centre may ask us to contact you about donating stem cells.
If we reach out, you could be the patient’s only match. It’s natural to feel both nervous and excited. So we’re there to help you every step of the way. We’ll start by checking if you are available and still willing to donate stem cells, and answer any questions you may have at that early stage.
If you are willing and available, we will ask you to complete a health screening questionnaire, and to go to a Canadian Blood Services site (or a nearby community lab) to provide blood samples to test for infectious diseases. We also arrange for blood samples to be sent to the transplant centre, so they can confirm you are an HLA match for their patient.
It could take a couple of months for the transplant centre to confirm you’re needed to donate stem cells. They may be assessing more than one potential donor to assure the best match, or the patient’s condition could change so that stem cell transplant is no longer an option.
If you’re confirmed, we’ll arrange for you to have a complete physical exam at the hospital where you’ll donate stem cells. You’ll also have a case manager to guide and support you throughout the donation process.
All tests beyond the buccal swab are only required if you’re matched to a patient and willing to donate stem cells when asked.
When you donate stem cells as a registrant with Canadian Blood Services, your personal information is not shared with the recipient. Stem cell registry donors and their recipients may only have contact with one another with mutual consent, and even then, no identifying information is shared until at least one year after the transplant. If your recipient is outside Canada, additional rules in their country may affect when or if they can have contact with you.
Donors and recipients always have the choice to remain anonymous.
A more diverse stem cell registry helps us make more lifesaving matches
Because HLA characteristics are inherited, some patients are fortunate to find stem cell matches within their own families. In a sibling, there is an approximately one-in-four chance of an ideal match. But the many patients who do not have suitable family matches must rely on the stem cell registry.
Since HLA types are similar in people with shared ancestry, a patient’s best hope of a match may be a registrant whose ethnic background is similar to their own.
“These are HLA associations based on how humans have clustered and migrated over millennia,” says Dr. Seftel. “For example, certain shared HLA types are more likely to be found in people of African origin, or of Southeast Asian origin.”
A bigger and more diverse stem cell registry can make more lifesaving matches possible. Currently, people of Indigenous, Asian, South Asian, Hispanic, Black, and mixed-race backgrounds make up only about a third of registrants, which means patients of these backgrounds may struggle more to find a match.
Registration is open to those aged 17 to 35. After registering, you may be called to donate anytime up to age 60. So please, don’t forget to keep your contact information up to date by contacting us if it changes. If you’ve donated blood, plasma or platelets, and you have a donor account, you can also keep us informed by simply logging in to edit the section called “Your Profile.”


