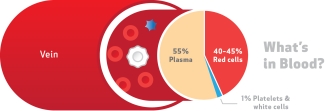
Blood is red. That’s because of the red blood cells or erythrocytes that whizz around your veins and arteries. The colour is a great visual marker, both clinically and emotionally, but sometimes its very redness hides the other important components that are in you to give. These include plasma, the straw-coloured liquid that carries red blood cells, white cells (leukocytes), other important molecules such as albumin, antibodies and coagulation factors, and tiny fragmentary cells called platelets.
What are platelets?
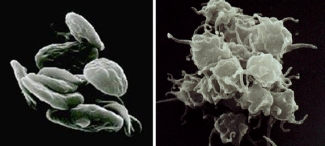
Platelets, or thrombocytes, are spherical cells (shaped like "plates"), much smaller than red or white blood cells. They come from megakaryocytes in the bone marrow, which release these tiny cell fragments into the blood stream every single day. An average adult makes around 1011 platelets on a daily basis to keep levels high enough for efficient blood clotting.
Yes — that’s 100 billion every day — why so many? Platelets are important for fixing the wear and tear our blood vessels experience every day. However, since platelets lack a nucleus, they only live for around 10 days in circulation, or up to 36 hours stored in the spleen. Hence, the constant production mode.
Why platelets? What do they do?
Platelets are an important part of hemostasis (stopping the flow of blood), which prevents you from losing too much blood when a vessel wall is damaged. Platelets help the blood clotting process (or coagulation) by gathering at the site of an injury, sticking to the exposed lining of the blood vessel, and creating a platform on which a clot can form.
Who needs platelets?
Patients with low platelet numbers (thrombocytopenia) can develop clotting deficiencies. Low platelet numbers occur if conditions either interfere with their production or accelerate their loss; severe bleeding such as from a road traffic accident or other trauma, drugs used in chemotherapy treatment, and even cancer itself are the most common reasons for this. Less commonly, conditions such as viral and bacterial infections, immune-mediated destruction, where a patient’s own antibodies attack platelets by mistake, or rare instances where the platelets created are faulty and cannot clot, also interfere with hemostasis.
Supply and Demand
Since low platelet numbers, through disease or drug treatments, trauma or surgery, compromise the clotting process and is potentially life threatening, patients often need a prompt infusion of donated platelets.
…and this is where donors come in.
Canadian Blood Services collects platelets from whole blood donations (by separating out the different components: red blood cells, plasma and platelets) and through apheresis donations.
Collection from a single donor, through apheresis, is very similar to regular whole blood donation, in that a cannula in your arm vein draws blood into a collection bag. However, instead of keeping all the components, only the platelets are retained. A centrifugation step separates the platelets from the rest, which then returns to the donor via the apheresis machine. For this reason, a platelet donation takes a little longer, around 90 minutes depending on the donor’s platelet levels but it can be repeated every 2 to 4 weeks.

Here a donor's platelets are being collected using the apheresis method. In this method, the apheresis machine is positioned next to the donor to extract his/her platelets and return the rest of their blood to their circulating blood.
Canadian Blood Services also prepares platelets from whole blood collections via a process called buffy coat collection. This process isolates platelets from red blood cells and plasma in a centrifuge at Canadian Blood Services manufacturing sites.
Managing the collection and distribution of platelets is a challenge and regular donation is vital for maintaining an adequate supply.

Platelets are extremely sensitive and they also need to be stored under gentle agitation to stop them from clumping. Furthermore, they need to be stored at room temperature, and for this reason platelet units are susceptible to bacterial growth. Ongoing research collaborations through the Canadian Blood Service’s research facility, netCAD, and scientists at other institutes are looking at ways to improve storage conditions for platelets to extend their shelf life . For example, platelets are usually stored in plasma; researchers have found that platelet additive solutions, rather than plasma, might be a better buffer for them since it seems to prevent cellular damage.
Other research collaborations look at how the transfusion service can assess platelet quality in storage, to give patients the best possible outcome. Researchers developed ThromboLUX, a laser device that transfusion staff could use to quickly and easily scan units for platelet quality. Using this information, clinicians can then choose the best suitable product to treat the patient in an emergency.
Platelets are in you to give. If you’d like to become a platelet donor, check out the resources below.
Further reading:
Blood for Research: Donating at netCAD
A Platelet Podcast: 'Platelets Unplugged: The Sticky Truth, a co-production of the International Collaboration for Transfusion Medicine Guidelines and the AABB, is the first in a series of ICTMG podcasts digging into best practice for the transfusion medicine community and health-care professionals.
Canadian Blood Services – Driving world-class innovation
Through discovery, development and applied research, Canadian Blood Services drives world-class innovation in blood transfusion, cellular therapy and transplantation—bringing clarity and insight to an increasingly complex healthcare future. Our dedicated research team and extended network of partners engage in exploratory and applied research to create new knowledge, inform and enhance best practices, contribute to the development of new services and technologies, and build capacity through training and collaboration.
The opinions reflected in this post are those of the author and do not necessarily reflect the opinions of Canadian Blood Services nor do they reflect the views of Health Canada or any other funding agency.
Related blog posts
Meet Dr. Elisabeth Maurer: she uses lasers to measure quality of platelets
" The ever-present need for innovative ways to combat dengue and other emerging viruses and pathogens has never been clearer."

