Aaliyah’s army: How blood donors helped one child survive during a pandemic
Canadian Blood Services continues to supply red blood cells to match her unusual blood type.
In spite of the pandemic sweeping the globe this spring, blood donors from across Canada selflessly ventured out to save the life of a five-year-old girl.
Chances are, those donors will never meet Aaliyah Mchopanga. But they are linked to her, and to each other, by a blood type that’s highly unusual among donors in Canada. And because of their donations, the medical team at BC Children’s Hospital had the crucial blood components they needed to save their patient.
Their generosity also made it possible for Aaliyah to meet a new baby sister, who was born on another floor of the same hospital complex where she was fighting for her own life.

Aaliyah Mchopanga with her sisters Naila, left, and baby Mya. Mya was born at the end of March while Aaliyah was in hospital because of health crises related to sickle cell disease.
A shocking diagnosis
Aaliyah’s father Abdi Mchopanga came to Canada from Tanzania in 2017 to study for an MBA at the University of New Brunswick. In 2018 he and his wife, Aziza Mfaume, settled in Surrey, B.C., with Aaliyah and her sister Naila, who is now eight.
The family was excited to begin a new life in Canada, but “after half a year, everything was upside down,” said Mchopanga.
When they arrived, Aaliyah’s parents had no idea she had sickle cell disease. People with this hereditary disorder have atypical hemoglobin molecules. That abnormal hemoglobin causes the usually round red blood cells to distort into a sickle, or crescent, shape which can get stuck in blood vessels. Patients can suffer painful episodes, anemia and organ damage.
Some of the first hints of a problem appeared during Aaliyah’s first Canadian winter.
“She was so excited,” said Mchopanga. “I think it was around January and there was snow. She spent most of her time outside, playing in the snow. [But] when she got in, she started crying and touching different parts of her body, complaining it was hurting.”
Cold temperatures are a known trigger for pain crises in sickle cell patients. The family received the devastating diagnosis that same winter.
“That was a very bad moment, knowing that your daughter is going to live with pain from sickle cell [disease],” said Mfaume.
The discovery was a particular shock because Mchopanga had no idea he was a carrier of the genetic mutation that causes the disease. To make matters worse, Aaliyah’s older sister Naila was diagnosed as well, though so far she’s been spared severe symptoms.

Dr. Gwen Clarke is a hematopathologist and the head of Canadian Blood Services’ Rare Blood Program.
The search for blood donors
Red blood cells from healthy donors are frequently key to health and quality of life for sickle cell patients. But finding donors for Aaliyah is difficult. She needs blood that matches not only her ABO blood group but her unusual combination of antigens — molecules on the surface of every red blood cell in her body.
It’s a common challenge for sickle cell patients in Canada, according to Dr. Gwen Clarke, a hematopathologist and head of the Rare Blood Program at Canadian Blood Services.
“That’s partly because most donors are white, and most sickle cell patients are Black,” said Dr. Clarke. “People of different ethnicities have different antigen combinations.”
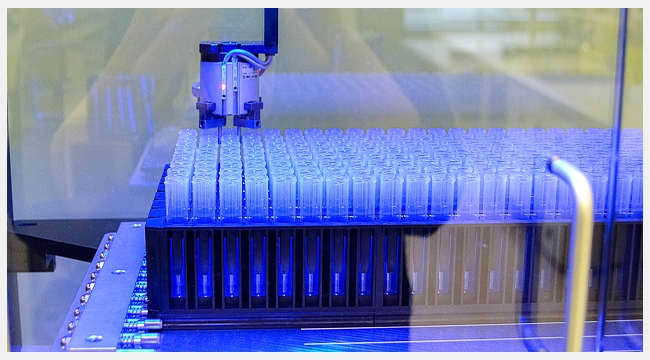
To meet the needs of those patients and many others, Canadian Blood Services encourages people from diverse communities to become regular blood donors. It also targets some donations for tests that look beyond what Dr. Clarke calls the “big 11” antigens to help patients who need a more precise match.
If you’ve donated blood more than once and also identified yourself as part of a non-Caucasian ethnic group, your blood is more likely to get the extra scrutiny that could see it directed to patients like Aaliyah.

Dr. John Wu is a clinical hematologist at BC Children’s Hospital in Vancouver, B.C.
Aaliyah’s army
To survive the spring, Aaliyah required blood from a small army of these thoroughly screened donors.
“She has to be one of the most challenging sickle cell anemia patients I have encountered in my almost 27 years here at the [BC] Children’s Hospital,” says Dr. John Wu, a clinical hematologist who first met Aaliyah in March 2019.
Dr. Wu became aware that Aaliyah’s blood type was unusual even among Black donors after she suffered an immune reaction to her second transfusion in late 2019. Soon after, the Rare Blood Program got involved. Canadian Blood Services staff worked to identify more than 70 donors in multiple provinces who could be contacted to help meet her future needs.
Dr. Wu recommended a program of red cell exchanges to begin in January 2020. Those would replace Aaliyah’s red blood cells with new ones from as many as four donors every few weeks.

Aaliyah Mchopanga, centre, with her father Abdi Mchopanga, right, and registered nurse Kate Douglas. Aaliyah regularly receives healthy red blood cells from donors to replace her own, which are affected by sickle cell disease.
At the edge of knowledge
Bringing in so many matching donors is a challenge, but a familiar one for Dr. Clarke and her colleagues at Canadian Blood Services. In cases like Aaliyah’s, “we basically have a group of donors that are almost on a recruitment schedule, where we go back to them and try to make sure they have appointments booked in the two to three weeks leading up to her transfusions,” said Dr. Clarke.
The effort heavily involves Canadian Blood Services’ National Contact Centre, the centralized service at the end of the 1 888 2 DONATE hotline. Members of the public contact the centre for information and to make appointments to donate, but the team also reaches out to specific donors as needed.
“We have case managers that are working with our National Contact Centre to say, ‘O.K., here’s a list of ten donors. Can you make sure that at least four of them have bookings in the next month?’” said Dr. Clarke.
Aaliyah’s need quickly ballooned, however, when she developed a complication that required additional transfusions as often as once a week. Then in mid-March, she suffered two strokes, the result of a rare syndrome affecting blood vessels in her brain. At one point, Dr. Wu said he reached out to a prominent hematologist who had published extensively on stroke in sickle cell patients. The news was disheartening.
“He said, ‘You have to tell the father that you’re at the edge of knowledge. Nobody knows what to do,’” Dr. Wu said.
Aaliyah’s condition soon led Dr. Wu to recommend the removal of her spleen. This high-risk procedure would require a supply of even more blood from donors.
She was still recovering from that operation when a bleeding ulcer caused her to lose the equivalent of her entire blood volume in a single day.

Louise Ringuette is a case manager with Canadian Blood Services’ Rare Blood Program.
Helping through a pandemic
It took massive transfusion to get Aaliyah through that last dangerous episode. Dr. Wu described her six-week hospital stay as “a very harrowing time for [her] mom and dad.”
The pandemic made it even more difficult, as Mchopanga worried about its potential impact on the supply of blood for his daughter.
“My question was, ‘What’s going to happen when people are not supposed to go out? That will include donors, right?’” Mchopanga said.
At the same time, Aaliyah’s plight was also weighing heavily on the minds of staff at Canadian Blood Services. Crisis after crisis forced Aaliyah’s doctors to continually draw down the small bank of matched blood. At the same time, the pandemic was forcing mobile donor centres to close, curtailing options for all donors, including Aaliyah’s matches.
Across the country in New Brunswick, Aaliyah’s case manager in the Rare Blood Program also shared Mchopanga’s fear that donors for Aaliyah would be too afraid to leave their homes.
“Every morning I would come in and wonder, ‘What’s happened with my case? Did they get any more donors?’ I’m getting worried,” said Louise Ringuette, a medical laboratory technologist. “When is she going for surgery? How is she doing?”
“It was very emotional, even just sitting behind a screen.”
A team united behind patients
In the end, Canadian Blood Services met Aaliyah’s need through national teamwork. Throughout her hospital stay, Ringuette kept in frequent contact with Rare Blood Program colleagues as well as Canadian Blood Services’ distribution centre in Vancouver. There, a technical specialist was keeping a close eye on the supply of matching blood across the country.
Blood can be shipped from any location in Canada, but staff also worked hard to recruit donors in Aaliyah’s geographic area to minimize any risk of shipping delays. They also froze some units of red blood cells, so Aaliyah could have those if fresher ones were in short supply. She needed some of those units this spring.
Sometimes helping a patient also takes a human touch. At one point, Ringuette and a colleague made the decision to share a few details of Aaliyah’s case with those who were calling prospective donors.
“We decided together that we should let National Contact Centre staff know that these efforts were for a young child, and because of COVID going on, to really stress the fact that she is in desperate need of these units,” said Ringuette. “I think that really helped with getting donors coming in at such a strange time.”
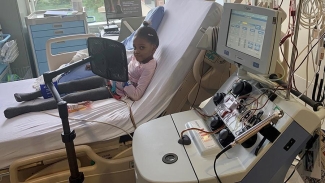
Aaliyah Mchopanga receives regular red cell exchanges to manage sickle cell disease, an inherited blood disorder.
Donors are a big part of the reason Aaliyah is now back home with her family, including a new sibling.
Aaliyah was asleep when her mother, who was visiting her in the hospital, realized she was in labour. Mfaume was admitted to BC Women’s hospital — which is part of the same hospital complex as BC Children’s — and delivered Aaliyah’s sister Mya on Mar. 29.
While Aaliyah gets to know her new sister, she is also going through rehabilitation to help her recover from the strokes she experienced. She also returns to the hospital every few weeks for more red cell exchanges. Her father praises the “wonderful people” on the hospital’s apheresis team, who are helping her adapt to the four-hour procedure.
“For a five-year-old who likes to play with dolls, it is difficult. She has to sit still the entire time,” he said.
Dr. Wu says he’s “very optimistic” about Aaliyah’s future with the disease. He said regular red cell exchanges have the potential to keep her in good health, and in the future, he’s hopeful a stem cell transplant or gene therapy could one day provide a cure.
‘An opportunity to dream’ for one young woman with sickle cell disease
The amazing journey of donated blood
Meantime, Aaliyah’s parents are so grateful for the care she has already received, including the gifts of blood donors.
“They are wonderful people, and we appreciate all that they do,” said Mfaume.
“I wish we could know them in person,” said Mchopanga. “The specific Canadian Blood Services team, our donors. But I know it’s a collective effort, and we can only say, thank you so much.”