International meeting sets research agenda for changing eligibility for MSM blood donors
Wednesday, February 01, 2017 Isabelle Robillard
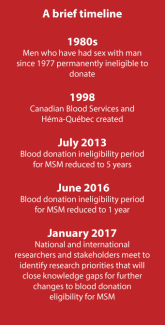
A two-day meeting held January 2017 brought together national and international stakeholders to identify research priorities for closing knowledge gaps that impact donor eligibility for men who have sex with men.
The issue
Blood and plasma donor eligibility is a complex thing. It is particularly complicated when it comes to men who have sex with men.
Donor screening represents one layer of safety that blood operators have implemented to ensure a safe blood supply for patients. Health Canada requires Canada’s blood operators — Canadian Blood Services and Héma-Québec — to file robust submissions to make any changes to procedures for screening blood donors. These submissions must be evidence-based and demonstrate that the changes will maintain the safety of our blood supply while providing benefits to the blood system.
Submissions to Health Canada must include: scientific evidence; quantitative risk assessment; potential impact on supply; potential impact on compliance of blood donors to the new screening question; IT changes and validation of the changes; training of staff; public perception and impact on overall safety of the blood system; stakeholder perspectives; and post-implementation surveillance.
The case for change
A lot of people ask us why we don’t screen potential donors individually. It seems simple, right? A person in a long-term same-sex monogamous relationship should be considered low risk and therefore eligible to donate. But, unfortunately, it’s not that simple.
The scientific evidence base currently available is inadequate. Most public health research has focused on men who have sex with men with behaviours that are considered high risk for infectious disease. This is the evidence that informs current regulations. New research must be done to generate the evidence required for low risk groups to be identified and included as eligible donors without introducing more risk to blood safety.
The meeting
To explore the possibilities and determine what must be done to evolve the current screening process — one that many perceive to be discriminatory — Canadian Blood Services, in partnership with Héma-Québec and with financial support from the Government of Canada, brought together experts from Canada and around the world for a two-day meeting. The aim was to share current knowledge and to set out the research priorities needed to inform future change for blood donation eligibility for men who have sex with men.
The research meeting included researchers from various disciplines, representatives from blood operators from around the world, Health Canada, as well as stakeholders representing patients receiving blood products, and members of the LGBTQ community.

Opening remarks
The meeting began the morning of January 24. Following introductions, the first to speak was Randy Boissonnault, Member of Parliament for Edmonton Centre, and a special advisor to the Prime Minister on LGBTQ2 issues.
His message was very clear: changes in the deferral policy in the last few years have been important but it is not enough and new scientific evidence could allow us to move towards more inclusive blood donor screening policies. With the current one-year deferral, we’re in line with most blood operators around the world. But, he challenged, what can we do to lead the way?
It has been a platform component for our government — driven by young Canadians across the country — to support plans that work towards blood donor policies that are as flexible and inclusive as safety allows, so that as many Canadians as possible can give blood. That is why we've committed $3 million to fund the research to make our blood system safe and inclusive for all.
- Randy Boissonnault, Member of Parliament for Edmonton Centre
Dr. Graham Sher and Serge Maltais, heads of Canadian Blood Services and Héma-Québec respectively, followed and set the goals for the next two days.
As Dr. Sher said, this is a deeply sensitive and emotional issue that cuts as close to matters of science as it does to matters of identity.
He explained, "The organizations involved in this meeting committed to sharing international practices and policies, identifying key research questions and projects, as well as barriers to that research, exploring partnerships for research, establishing processes for applications and, finally, for granting of the research funding that has been made available by the Government of Canada."
Representatives of patient groups and of LGBTQ organizations then shared their perspectives. From the patient perspective, the safety of the blood supply remains the top priority closely followed by the sufficiency of the supply.
The stakeholder engagement process that Canadian Blood Services has spearheaded and been committed to has helped build the trust we have in Canada’s blood operators. For individuals living with Primary Immunodeficiency and on Immunoglobulin replacement therapy, one treatment contains the antibodies of thousands of donors and can be administered every three to four days. Quickly, that could represent 24,000 donors per year, or one million donors for 10 years, and it’s a lifelong treatment. This consultative process is crucial. Creative solutions likely exist, such as lifting the deferral policy for donations of plasma for fractionation. In this case, donations can be quarantined to allow for longer testing periods, and we know that the fractionation process inactivates pathogens in a highly effective way, thus reducing the risk for recipients.
-Richard Thompson, CEO, Immunodefficiency Canada
With LGBTQ organizations, there remains a perception that the current donor eligibility criteria are discriminatory. And, that all Canadians want the same opportunities to contribute to society.There was a general feeling that grouping all men who had sex with men in one population risk category for donor screening purposes had the unintended consequences of falsely painting them all with the same brush, when the reality is that not all men who have sex with men practice high-risk behaviours.
It is crucial that researchers work with LGBTQ communities to keep communities informed of progress and to ensure they understand the research goals and results, and that the research at all stages be conducted in an open and transparent manner.
-Kathleen Pye, Director, Research and Policy, EGALE Canada Human Rights Trust
The workshop
A review of current international practices and available data was shared by experts from around the globe including the U.S., New Zealand, Australia, England, Germany, France, Italy, Spain and Portugal. This was an interesting session as it allowed the review of various approaches to donor screening and their impact on the donor pool, blood safety and how blood operators operate.
Participants — researchers and stakeholders alike — then formed smaller groups to dig into what research is needed to move forward and what research projects may actually look like. The breakout rooms were abuzz with energy and passion.
Breakout groups later presented their findings and together next steps and priority research areas were determined.
Some of the identified research priorities include:
- Research to inform the development of an individual risk assessment donor policy (behavioural based) or to strengthen the existing policy (population based).
- Research to evaluate operational feasibility of potential donor deferral policies and their acceptability.
- Risk modelling and surveillance to assess the risk associated with alternative donor selection policies.
All in all, it was an extremely productive experience. One that led to a better understanding of the issues around deferral policies for blood donors who are men who have sex with men and to the establishment of new collaborations among researchers, regulators, blood operators and stakeholders.
Our next step is now to facilitate the completion of meaningful research projects that will generate the data we need to make a change based on evidence. With funding from Health Canada, a new competitive MSM Research Grant Program is being launched.
The program’s official objective is “to ensure the generation of adequate evidence-based research for alternative screening approaches for blood or plasma donors, which could evolve the current deferral policy for men who have sex with men while maintaining the safety of the blood supply.” It’s open to Canadian researchers and promotes collaborations with stakeholders.
Canadian Blood Services – Driving world-class innovation
Through discovery, development and applied research, Canadian Blood Services drives world-class innovation in blood transfusion, cellular therapy and transplantation—bringing clarity and insight to an increasingly complex healthcare future. Our dedicated research team and extended network of partners engage in exploratory and applied research to create new knowledge, inform and enhance best practices, contribute to the development of new services and technologies, and build capacity through training and collaboration.
The opinions reflected in this post are those of the author and do not necessarily reflect the opinions of Canadian Blood Services nor do they reflect the views of Health Canada or any other funding agency.
Related blog posts
A two-day meeting will be held in January 2017 with national and international stakeholders to identify research priorities for closing knowledge gaps that impact donor eligibility for men who have sex with men.
“It’s in you to give" is the fantastically simple call to action from Canadian Blood Services. But for some people — such as those of us with a mixed bag of travel and medical histories — it isn’t so easy to just show up, roll up (a sleeve) and then settle back as this life-giving liquid flows into...

